Dogma, Physiotherapy, and the Sociopolitical Field
taking a step back

As an aspiring clinician, I felt pressured to become familiar with the field’s foundational concepts, and to be a skilled follower of its basic tenets. Much like converting to a new religion, physiotherapy calls us to ‘abandon a corrupt set of beliefs … and then with the force of revelatory discovery, to be moved into the the light of truth’ 1 We are stripped naked and baptised in the presuppositions of our profession, becoming One with those who came before us, knowing what they know so that we can pick up the baton and “further the profession.” We quickly specialise, settle on an identity within physiotherapy, define our clinical practices, and find our guru(s). We find ourselves thrust into the epicenter of the sociopolitical field without the chance to reckon with the structure of it. The sociopolitical field in which physiotherapy has come to find power and credibility is made imperceptible.
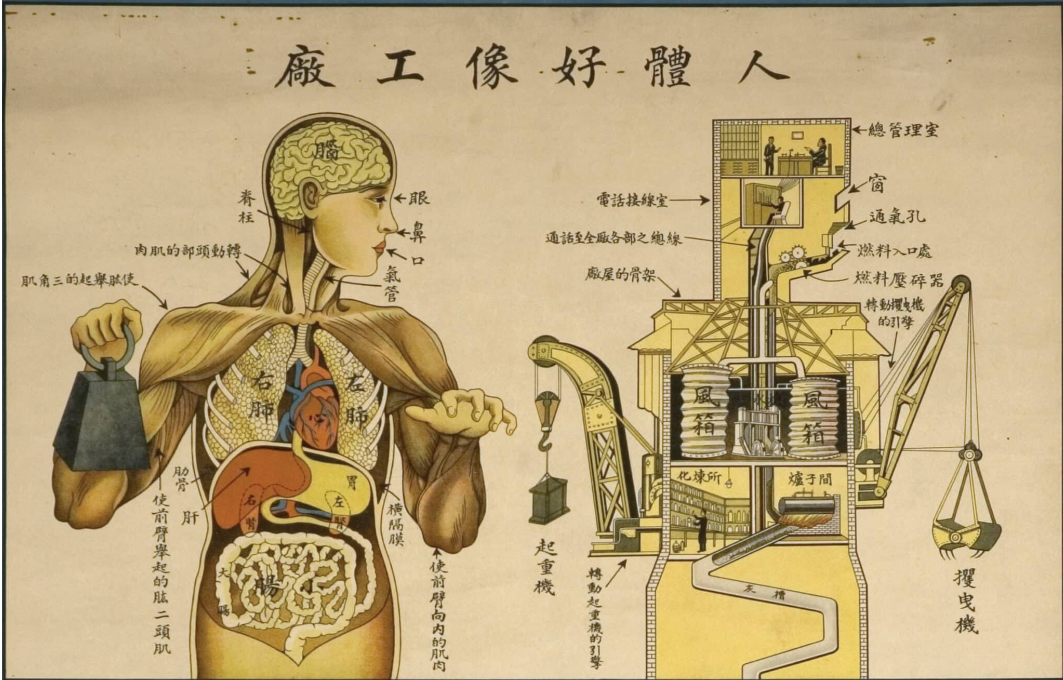
The sociopolitical field is seldom adequately addressed in healthcare education - both clinically and practically. While the emphasis on the lived phenomenological aspects of health have gained prominence, there still exists an epidemic of widespread neglect of the sociopolitical field. To consider and critique the sociopolitical is to critique the system in which our profession is nested. Neglecting the sociopolitical is partly intentional and partly a symptom of the system itself. A medical profession which brings the messy entrails of the sociopolitical (neoliberal / capitalist) field to our conscious awareness risks its own destruction. That which no longer serves the agenda of the sociopolitical system, a profession which escapes the territory of the major, is always at risk of being recaptured, destroyed, and reabsorbed.
It is as though our noses are pressed up against a painting, accepting the belief that the closer we are the more clearly we can see. Our time is occupied by discerning the different shades of yellow right in front of our eyes. When we attempt to step a way, making some space between ourselves and what we are seeing, we are pushed back into it, encouraged to look even closer.
Physiotherapy’s preoccupation with (for the most part) the biological and minor aspects of the psychological, limits our perspective. The passive adoption of the profession’s presuppositions with no critical eye for the system it serves, conforming to predominant thought, puts us at risk of only being able to think of the profession in a limited number of ways. It is this unreflective adoption of seemingly self-evident presuppositions and clinical dogmas, that, transferred to us through recognition, stifles or even halts thought. We become one of the many; our ability to recognise and repeat; recognise and regurgitate, allows us entry. Entry into a world - or a profession - in which we can no longer bring forth anything new. Physiotherapy has formed, what french philosopher Gilles Deleuze would call, its own Dogmatic Image of Thought which has stopped us from thinking.
There is a more or less implicit, tacit or presupposed images of thought which determines our goals when we try to think. — Deleuze 19952
But before we address the sociopolitical field we first need to untangle our presuppositions on which the sociopolitical field stands. To do this requires us to consider how we use recognition to construct thought.
Recognition
For Gilles Deleuze, thinking has primarily been considered an exercise of recognition, defined as “the harmonious exercise of all the faculties upon a supposed same object.” 2 A thinker recognizes an object when they use their faculties of memory, perception, understanding, and judgment in a concordant manner upon the object. “Ah-ha yes of course, that makes sense” is the comfortable feeling that we experience when we see a connection that strikes us as right. Something “clicks,” we say 1.
Recognition, however, isn’t the full picture. In order to recognize, we need what Deleuze refers to as representation. To be able to “recognize” a thing, it needs to represent the thing in thought. I.e, to recognize a chair, I need some understanding of the representational category (or ‘blueprint’) of chairs and its place within our current social linguistic system. Certain essential characteristics help us recognize the object. A rudimentary example might be that a chair has four legs, a place to sit, and it often has a backrest and/or arm rests. This enables us to come across an object we may have not ever seen before, but to still recognize it as a chair.
This representational model of thinking is a powerful ‘construction’ that is practically and theoretically useful, bringing about some sense and order to the world. Large parts of our daily life are taken up by acts of recognition, as we seek to understand or “get” or perceive what is presented to us. I can see a tree I have never seen before and with a high level of certainty know that it is a tree. When I come across a building with a big red cross and ambulances, I recognize it is a hospital. When I see someone running next to the road, I recognize he is not running from or after something but rather within our particular social context he is exercising. Recognition is valuable within healthcare; we try to recognize a client’s clinical presentation, diagnosis, best treatment pathway, psychological barriers, and so on.
In the same way, to be able to recognize an achilles tendinopathy, we need to determine through our perception if it has the requisite essential features of a tendinopathy to determine if it reflects our representational category for an achilles tendinopathy. This is based on our memory of previous examples of this condition. This means we need some understanding of the representational category of achilles tendinopathies within our healthcare system of meaning. If recognized, we will feel the satisfying feeling of “aha! I know what is going on here” surge up within us. The client’s variety of presenting features makes sense to us. We can deploy the category, which enables us to attend to them in the manner expected of us.
Crucially, this is what we begin to believe is emblematic of what it means to ‘think’ as a physiotherapist. “I am a good thinker because I could recognize and categorize what was presented to me”.
For Deleuze, the trouble comes when these representational categories and systems of meaning come to be understood as self-evident categories which simply ‘name’ a reality. In other words, they become Dogma and sustain a conformist image of thought. When we do not critically examine the underlying categories of representation, we consider predominant ideas, theories, principles, or values as “Reality” or “Truths” that are merely waiting to be “discovered.” The moment we think of something as understood, traditional, we are limited in thinking of it in that way. We are trapped in the conformist system of thinking and nothing novel can be thought.
When we see our presuppositions as “obvious” or “something everyone knows,” even if implicitly, we imply that they are set in stone, immovable, uncontestable. We imply that there exists something about the concept that does not merit the scrutiny we would normally apply. Deleuze calls this type of thought “common sense.” For him, this does not constitute real thought, only the dogmatic image of thought. This desperate need to cling to “common sense” and use it as the best point of departure for inquiry, is problematic for real inquiry.
Presuppositions will have the appearance of “everybody knows, no one can deny that…” This rhetoric has been used with countless presupposed beliefs within the profession including the belief that joints become painful due to accumulated wear and tear over time 3, degenerative changes in the spine found on radiological imaging indicate the site of a client’s pain 45, back pain is due to non-ideal posture 678, scapula dyskinesis being reliably related to shoulder injuries 9 and so on.
The Sociopolitical Field
The trouble with this Dogmatic Image of Physiotherapy is that the larger systems (historical, political, and socioeconomic fields) upon which our particular representations are contingent are often neglected. Put another way, we bypass the historical and socio-political character of the existing categories of representation and perpetuate their unquestioned validity. When this occurs, the dominant Thought appears to simply reflect reality; we view it as a transcendent Truth that we can apply to the world at large.
The specifically dogmatic character of the traditional image of thought can therefore be discerned in the manner in which acts of recognition are taken to be emblematic of what it means to think, acts of recognition that are dependent upon representational categories that, in order to be understood as simply naming or mirroring reality, are taken to be transcendent, transparent and self-evident categories rather than historical, socio-politically embedded constructions. — Roberts 201310
Crucially I want to draw attention to the dominant lens through which we view health, the biopsychosocial model. The taken-for-granted presuppositions might be the social, historical, economic, and politically contingent representational categories surrounding the biopsychosocial model. Clinicians wield the biopsychosocial model under the guise of “holistic care,” but often ignore its (or their) own enmeshment within a neoliberal socio-political field which stymies holistic care. Placing the onus of responsibility on our clients may seem like “common-sense” and self-evident. We might say “No one can deny that patients need to foster self-efficacy and less reliance on medical providers.” We think individual responsibility is empowering in all cases. However, this is deeply political and quite recent.
During his 1981 inaugural address, Ronald Reagan asked “if no-one among us is capable of governing himself, then who among us has the capacity to govern someone else?” With this statement, he outlined his complex political-economic agenda to shift responsibility from the state to the individual. These policies, mindsets, and cultural shifts have been further developed through the politics of Bill Clinton in the U.S. and Tony Blair in the U.K. The pervasive rhetoric of personal responsibility has altered the role of the government, whose primary role now is to facilitate the conditions in which citizens can take on more responsibility. By strongly focusing on the individual and by disregarding the importance of community and state, neoliberalism increases the importance of individuality while decreasing the importance of society or governance. Think of the messaging around climate change for example - politicians preach “stop buying straws!” while much less is said about the larger corporations which profit from the continual production of environmentally harmful products. Healthcare is not absolved of this rhetoric.
When left unchecked, the biopsychosocial model reduces all three domains (bio, psycho and social) to the responsibility of the individual and away from society, larger systems, and even clinicians. When we discuss the biological, we discuss it in the context of our clients’ ability to affect their biology through exercise and “compliance” with treatment. When we discuss psychology, we identify the individuals’ maladaptive psychological state (poor self-efficacy, fear avoidance behaviour, pain catastrophizing) and administer interventions which aim to assist them in realising and correcting their said psychological deficits or maladaption. Perhaps most tragic of all, when discussing the social domain, we haven’t a clue what we are doing. The best we can come up with is a limp attempt at discussing their social relationships and how they are socially supported. If we decide that their social support structure is not adequate, we make recommendations to the client on what they might consider doing to remedy the situation. God forbid you ask a physiotherapist to venture close to questions of economic security, discrimination, or acces to services or infrastructure 11. One of the overarching aims of healthcare is to hand the person’s health over to the individual and out of the hands of the state. Individual responsibility can be useful and important too, but it is a thin slice of the pie.
To assume the biopsychosocial model - or whatever model, treatment modality, or diagnostic label we were taught - represents a “Truth,” and not a reflection of the socio-political field we are steeped in would be remiss.
If the contingent historical and socio-political factors which construct the biopsychosocial model are elided, if its representational category is understood as transparent and self-evident, mirroring or reflecting the way in which health exists in the world and has been waiting to be discovered, then the biopsychosocial model, would largely be understood as uncontroversial and unproblematic. This is clearly not the case. We could say the same for many taken-for-granted concepts such as Pain Self-efficacy, Perceived Injustice, Postural Alignment, “pain as a response to threat”, and so on. We often come against the limitations of these Dogmas when we are dealing with the complexity of a patient, intersecting across a variety of social, economic, physiological, and psychological fields. When we treat these concepts as Dogmatic Images of Thought, we foster unreflective acceptance of existing categories and acts of recognition. This stifles our ability as clinicians and critical thinkers in the field.
The form of recognition has never sanctioned anything but the recognisable and the recognised; form will never inspire anything but conformities. — Deleuze 19952
We can keep ourselves quite occupied negotiating and swapping out some “Truths” for better ones (i.e. the biopsychosocial over biomedicine; etc.) We might think we are trading one faulty representation of reality for a more accurate one, but what we are really trading is a complex set of beliefs contingent upon socio-political and historical factors which suit our particular worldview and cultural milieu of the time.
When we take a step back from the profession, creating space between ourselves and the “painting” as it were, we can question what it was that we were looking at. We see the painting as a whole, situated in a context; the frame within which the painting sits, the wall on which the painting hangs, the building wherein the painting is kept, the people who have access to the building, and so on.
Critique and Resist
We might understand Deleuze’s critique of the Dogmatic Image of Thought as a warning against intellectual complacency or dogmatism. We cannot say that when we are engaged in an act of recognition, when we are engaged in “what everyone knows” that thinking is occurring. What of wonder and the sublime? What of the new and the things unthought? As Deleuze asked: “who can believe that the destiny of thought is at stake in these acts, and that when we recognise, we are thinking?”
Thinking creatively and eliminating presuppositions at the starting point of thinking will move us beyond the bounds of the Dogmatic Image of Thought. Within physiotherapy, this means becoming aware of our profession’s predominant, favoured ways of thinking.
Once we have become aware of our go-to assumptions, how do we create new concepts or categories that liberate us from dogmatic thought?
Deleuze suggests, “the conditions of a true critique and a true creation are the same: the destruction of an image of thought which presupposes itself and the genesis of the act of thinking in thought itself.”2
It starts with an ongoing critique of the meaning of a given representational category that has gained predominance. We need to critically analyse our profession’s imobile categories and how they were constructed in response to a diversity of theoretical and practical problems that were deemed important to a particular historically embedded socio-political milieu 11. By reflecting upon the historical and socio-political function of the category, we seek to determine the value of the ongoing adherence to and employment of that category. Only on the backbone of this critique, can we start to experiment with these categories within the current historical and socio-political milieu. We might even creatively transform them by integrating new concepts into our practice, and curiously analyse what value each concept might have for the everyday concerns of the clinician.
Deleuze’s work inspires a solution, a manner in which we escape the Dogmatic Image of Thought. When we are implicitly presented with the presupposition “as we all know…”, resist. Deleuze suggests that we should refuse to be represented as one of the everybody. Disallow others to speak on our behalf and instead say “I am not part of the big everybody”. All of what has been presupposed once again returns to philosophical scrutiny. This is where real thought can begin. When called to recognise, choose rather to re-cognise, think again, go deeper, look behind “common sense”.
References
-
Burbules, N., 2000. Aporias, Webs, and Passages: Doubt as an Opportunity to Learn. Curriculum Inquiry, 30(2), pp.171-187. ↩︎
-
Deleuze, G., 1995. Difference and Repitition. Columbia University Press. ↩︎
-
Alentorn-Geli, E., Samuelsson, K., Musahl, V., Green, C., Bhandari, M. and Karlsson, J., 2017. The Association of Recreational and Competitive Running With Hip and Knee Osteoarthritis: A Systematic Review and Meta-analysis. Journal of Orthopaedic & Sports Physical Therapy, 47(6), pp.373-390. ↩︎
-
Schmidt, C., 2017. Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations. manuelletherapie, 21(02), pp.54-55. ↩︎
-
Nakashima, H., Yukawa, Y., Suda, K., Yamagata, M., Ueta, T. and Kato, F., 2015. Abnormal Findings on Magnetic Resonance Images of the Cervical Spines in 1211 Asymptomatic Subjects. Spine, 40(6), pp.392-398. ↩︎
-
Pope, M., Bevins, T., Wilder, D. and Frymoyer, J., 1986. The relationship between anthropometric postural, muscular, and mobility characteristics of males ages 18–55. Clinical Biomechanics, 1(4), p.237. ↩︎
-
Nourbakhsh, M. and Arab, A., 2002. Relationship Between Mechanical Factors and Incidence of Low Back Pain. Journal of Orthopaedic & Sports Physical Therapy, 32(9), pp.447-460. ↩︎
-
DIECK, G., KELSEY, J., GOEL, V., PANJABI, M., WALTER, S. and LAPRADE, M., 1985. An Epidemiologic Study of the Relationship Between Postural Asymmetry in the Teen Years and Subsequent Back and Neck Pain. Spine, 10(10), pp.872-877. ↩︎
-
McQuade, K., Borstad, J. and de Oliveira, A., 2016. Critical and Theoretical Perspective on Scapular Stabilization: What Does It Really Mean, and Are We on the Right Track?. Physical Therapy, 96(8), pp.1162-1169. ↩︎
-
Roberts, M., 2013. Beyond the bounds of the dogmatic image of thought: the development of critical, creative thinking in the mental health professions. Journal of Psychiatric and Mental Health Nursing, 21(4), pp.313-319. ↩︎
-
Nicholls, D., 2019. End of Physiotherapy. Routledge. ↩︎